
Osteoporosis and Osteopenia
Osteoporosis is the medical term for bones that are demineralising (predominantly losing calcium but also losing other minerals) and are therefore at increased risk of fracture. A lower than expected bone density with no statistical increased risk of fracture is termed osteopenia.
This is a common problem affecting up to one in ten women after the age of 60 and one in three after the age of 70. Men can also have this problem, but at a lower rate. It is recognized now that many factors lead to fractures, not just bone density. Age, genetics, heredity, body weight, certain diseases, incorrect diet, lack of exercise and trauma all play important roles.
Diagnosis, Tests and Investigations
Diagnosis is often made, unfortunately, after a fall causes a fracture and X-rays indicate that the bone is thin. Regular X-rays are not the way to quantitatively assess bone density. This is done by using a specialised low-dose X-ray known as the DXA (previously known as a DEXA Scan) or Quantitative Ultrasound (qUS)
There are other techniques done at specialist centres such as
- Single Photon Absorptiometry (SPA),
- Quantitative computed Tomography (qCT) and
- Radiographic Absorptiometry (RA)
DXA/DEXA Scanning is considered the gold standard, with established clinical efficacy and only low radiation dose. It has very good precision & accuracy (sensitivity and specificity). The other tests are possibly less precise than DEXA, they tend to be more expensive and deliver a larger radiation exposure. (1)
The other tests are, possibly, less precise than DEXA, tend to be more expensive and deliver a larger radiation exposure. (1)
Dual-emission X-ray absorptiometry (DXA) measures bone mineral density (BMD). Two X-ray beams of different low intensity are aimed usually at the top of the femur (leg bone) in the hip and the lower spine (lumbar) vertebrae. The computer takes into account the density of the tissue of the leg, and determines, from the amount of X-ray that has been absorbed, the density of the bone. The results are compared to the expected density of an individual of the same age
Dual-energy X-ray absorptiometry is the most widely used and most thoroughly studied bone density technology. Statistically 68% of repeat scans fall within what is known as one standard deviation which can be the difference between normality, osteopenia or osteoporosis. Scanning machines vary from centre to centre and even within the same centre the same machine may show a marked variation on the same patient. We also know that exercise can rapidly increase bone density and so having a DEXA scan performed after, say, a 2-3 mile walk could lead to variability and influence accuracy (1a).
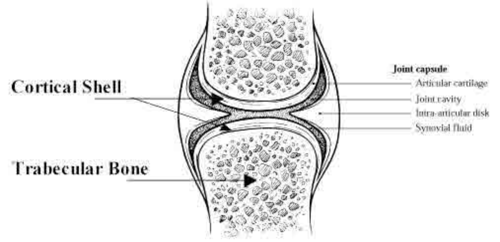
One major disadvantage of DXA is that it does not differentiate between cortical(outer) and trabecular (inner) bone so a thin inner bone may be hidden by a thicker less supportive outer plate.
Also, previously fractured bones or scans in those with spinal deformities may give inaccurate results.
Ultrasound
Changes in qUS of the heel (the area generally measured) may not reflect changes in BMD at the spine or hip.
However a review of studies suggest that qUS is a useful tool in determining fracture risk (2). There is some evidence that qUS of the heel can predict fracture risk of hip and spine independently of BMD measurements (3). qUS in addition to BMD evaluation by DEXA may give a better estimate of fracture risk than DEXA scanning alone (4).
Other tests
It is also important to rule out heavy metal toxicity, especially that of lead. This should, if possible, include white blood cell metal sensitivity testing as metals in bone may not show up in urine or faecal tests
DPD Urinalysis. This compound increases in the urine when bone is being broken down at a faster rate than it can be built. There is strong evidence that this sort of testing especially if combined with BMD scanning can predict risk of fracture even in pre-menopausal women.(5)
There are now investigations from simple blood analysis known as Genomic tests that can indicate who might be at genetic risk of osteoporosis and what dietetic, environmental and life-style changes might benefit a specific individual. OsteoGenomic test results need to be interpreted by a doctor considering the individual patient and their medical and family history.
Conventional blood tests, that are often grouped together, indicate increased bone ‘turn over’ or loss but do not really alter therapy choices. (These include Serum total alkaline phosphatase Serum bone–specific alkaline phosphatase, Serum osteocalcin, Serum type 1 procollagen (C-terminal/N-terminal), Urinary hydroxyproline, Urinary total pyridinoline (PYD), Urinary free deoxypyridinoline (DPD), Urinary collagen type 1 cross-linked N-telopeptide (NTX), Urinary or serum collagen type 1 cross-linked C-telopeptide (CTX), Bone sialoprotein (BSP), Tartrate-resistant acid phosphatase 5b).
Recommended Screening Investigations:
- DPD urinalysis
- DXA scan or for routine scanning Bone density ultrasonography (qUS)
-
Genomic Testing for optimising nutrition
A simple cheek swab sent to a specialist laboratory leads to a report that provides specific information regarding risk and diet preferences for any individual based on their genes.
This includes osteoporosis risk as well as detoxification capability, the requirement of increased vitamin & mineral levels, the likelihood of the presence of environmental toxins due to your innate detoxification capability, your ability to metabolise nutrients and many other areas relevant to optimising nutrition. Results within this test include the body’s ability to break down hormones including catecholamines involved in stress and, importantly, female hormones. This and methylation are genetically predisposed and specific supplements can increase metabolic function if needed.
You can read about the test here: https://nutritiongenome.com/experience-the-report The cost through my practice is £488 inclusive of administration and my overview (but not of my full summary which one of my nutritional clinical assistants can provide if required). As the report is well produced much of the information directing you to correcting your diet and to what nutrients to take is clearly written over 4 pages (p.31-34 inclusive) of the 89 page extensive Genetic Health Analysis report.
For those with established osteopoenia or osteoporosis investigate the above and also:
Consider investigating the above and also:
- Faecal and urine metal toxicity (as metals such as lead cause bone loss)
- White blood cell metal sensitivity
Treatment Options
Exercise
Muscle strengthening plays an equal or possibly greater role than weight-bearing exercise in the management of osteoporosis. Even walking may have benefits for bone mineralization and is the most affordable. Resistive exercises usually require light weights, isometric or minimally isotonic resistance such as compressible balls or cushions, or elastic bands. Weight-bearing exercises such as walking and jogging play a very important role in aerobic conditioning and can have a modest effect in the prevention of osteoporosis (15).
Lifestyle and Diet
Do not smoke. Excess alcohol (possibly only half of the standard health recommendation of more than 20 units a week in men and 14 in women) will adversely influence bone density.
Exercise benefits are enormous and one of the most important methods of increasing bone density is weight-bearing exercise. Weight-bearing exercise is simply walking carrying enough weight to be noticed but not muscularly taxing (a backpack with suitable weight, for example). Around 40 minutes a day is required if bone density is low and perhaps half that for prevention.
Under or overeating can interfere with bone metabolism, as can missing out on sunshine (for the vitamin D).
Review online calcium-rich foods and pick those you like and eat more of them. Although there is controversy, cow’s products may not be the best things for bone stability according to some authorities (16)
A more alkaline diet is of importance. Please review the following link for more information. http://www.osteopenia3.com/Diet-for-Osteopenia.html and also consider making this sauerkraut a part of your weekly menu: http://recipes.mercola.com/raw-sauerkraut-recipe.aspx and select some alkaline juice recipes for smoothies etc https://www.google.co.uk/webhp?sourceid=chrome-instant&ion=1&espv=2&ie=UTF-8#q=alkaline%20juices%20recipes
The importance of bowel flora (the gut microbiome) is very much underestimated. This link explains things well: https://chriskresser.com/the-microbiota-and-bone-health-yet-another-reason-to-protect-your-gut/
Milk may not benefit bone density. This paper states…. “we concluded that a greater intake of milk and dairy products was not associated with a lower risk of osteoporosis and hip fracture.” (16a) Fuller proof can be read in this book: https://viva.org.uk/materials/white-lies/
Avoid Oestrogen pollution
Harmful oestrogens are abundant in our water supply due to their being taken by the female population as the oral contraceptive pill and then urinated into our water supply. Many industrial processes form oestrogens that are leached into our water supply, soil and our atmosphere and one of the worst supplies of oestrogens comes from heated plastics – even a sun-warmed water bottle may be a risk. The water we drink from taps, if not filtered through a reverse osmosis purifier, has the potential of being “bad for you”. Oestrogens can accumulate in the body especially if we genetically lack high activity in a process of detoxification called methylation – Oestrogenomic testing can advise us of that.
Some authorities note that the highest levels of osteoporosis are found in the Western world where more milk is drunk and more oestrogens are ingested unwittingly (14).
On that point, fat tissue makes natural oestrogens and thinner post-menopausal women have a slightly higher tendency towards osteoporosis than those with a certain amount of fat. Too much fat unfortunately leads to an increased risk too.
Conventional Drug treatment
Please go online and complete the FRAX form to see if you fall into the category of high risk. https://www.sheffield.ac.uk/FRAX/tool.aspx?country=9
If not stick with naturopathic options for as long as possible.
Conventional treatment principally uses drugs known as bisphosphonates. These are generally considered when someone is at a high risk of fracture. All of these, unfortunately, have potential side-effects. Alendronic acid is the most common one used here in the UK and adverse effects can be very serious particularly the development of jawbone necrosis (death of tissue) (6). There are well established potential risks and side-effects including stomach ulcers, atrial fibrillation, and fractures in unusual sites as well as oesophageal cancer
This is often given in combination with pharmaceutical grade calcium and Vitamin D. Please see further comments on Vit D below. The mineral strontium is also being used in certain pharmaceutical developed drugs.
Special hormone replacement therapy drugs known as SERMs may be considered by experts as they have been shown to pinpoint their activity on bones (as opposed to other tissues where HRT may have an influence such as breast, skin, ovaries, etc.).
That said the conventional attitude is that, in the balance, the risks in the short term certainly, are currently less than the benefits from such drugs.
Calcium in Osteoporosis
The use of calcium carbonate, the most used and prescribed pharmaceutical source, is of little consequence in bone density and may carry a risk of reducing bone density due to various mechanisms (9a). In part calcium deficiency is quite hard to achieve for those who are not impoverished, and in part, many calcium supplements do not get to the bones and specifically calcium carbonate settles in the arteries increasing risk of heart attack (11)
This is because calcium that is found in nature is generally in a combination of calcium with phosphate molecules and therefore enters bones very easily. We have evolved receptors for this task.
A 1000 kg elephant needs up to 9 grams of calcium a day (10) This is obtained in ‘food-state’ form increasing availability – leaves, bark but particularly mud, and soil (when pulling grass). Our osteoporotic population (predominantly women over 60) weigh generally 1/50th of that of an elephant (if our metabolism were the same as an elephant that would equate to a need of 180 mgs. Current general advice from conventional medicine is to prescribe between 1200-2000mg daily of chalk (calcium carbonate).
Please watch this 5 minute video: https://www.youtube.com/watch?v=OD7T5GF6b28
Vitamin D deficiency is very common in countries where sunshine is not in abundance and has become a bigger problem since we have become scared of the sun because of the fear of skin cancers. It is extremely important to expose as much skin to as much sun for as long as is possible ensuring that the skin does not pinken, redden or, of course, burn. The actual dosage that is recommended for the average adult is, in most Vitamin D researchers’ and experts’ opinions, far below that which should be taken. Osteoporosis demands daily supplemental levels of 2000 IU or more (12).
Vitamin K is also required for bone assimilation as are certain amino acids (proteins) that are required to make the mesh upon which the calcium, boron, strontium and other required minerals sit.
Bioidentical hormone replacement therapy
Oestrogens are known to enhance bone density but, progesterone may also do the job. and do so more efficiently. As women go through menopause both these natural hormones diminish. The orthodox world can produce oestrogens from pharmaceutical sources that are accepted by the body without too many side-effects and risks. The same cannot be said for artificial progesterone. called progestins. Therefore, artificial oestrogen as HRT is often prescribed but progesterone is not, except in small doses to balance the oestrogen intake.
Bioidentical progesterone must be prescribed by a physician. bHRT needs to be taken trans- dermally (through the skin) or, better still but less well liked, sub-lingually (under the tongue). There are oestrogen and progesterone sensitive tumours (13) and so tests are required before and during prescribing bHRT (or any HRT) to promote safety first.
“In women, osteoporosis coincides with menopause. The hypothesis that progesterone and not estrogen is the missing factor was tested in a clinical setting and was found to be extraordinarily effective in reversing osteoporosis.”
https://tinyurl.com/2zdnakza
Stress and Osteoporosis
There is strong evidence that psychological stress effects bone density (13a).
Research has focused on the production and activity of stress hormones such as cortisol, epinephrine (adrenalin), and norepinephrine all of which can influence bone metabolism.
As in all conditions, but perhaps more so in such chronic and complex issues such as osteoporosis, Tai chi, Qi Gong and Yoga (all to a degree weight bearing) are so very important.
A good book to help guide you further can be obtained via this link: Book : https://www.amazon.com/Your-Bones-Prevent-Osteoporosis-Naturally/dp/1607660075.
Recommended basic supplementation:
Tricatione (- a natural nutritional supplement obtained from the aerial part of the Spring horsetail (Equisetum arvense), which is rich in vegetal silica, combined with a specific marine oily extract to enhance a better cell membrane penetration.)
https://www.labo-lestum.fr/excellence/tricatione-11.html
Bone basics – an equally potent supplement combination http://www.aor.ca/en/product/bone-basics
Collagen Hydrolysate - 2 scoops bd https://www.amazon.co.uk/Great-Lakes-Gelatin-Hydrolysate-Unflavoured/dp/B08CNLKFTJ
Flaxseed oil capsules 1000mg (90) - 1 bd - 2 pots - 29.00 https://edu.rsc.org/news/flaxseed-oil-and-healthy-bones/2020535.article
Amino acid supplementation to help the bone matrix formation upon which the bone minerals sit - preference is for Amino Spezial
Additional (to that in the supplements mentioned above) Vit D 5000 IU/ Vit K 200mcg daily
(**An alternative option to Bone Basics if faced with a poor benefit from is: Tisso Pro Osteo Complete – a bone supplement including plant extracts and supplements (12a) https://drive.google.com/file/d/0B8ToBiT4VsbiQ3pPWDJHa2N5dUE/view)
In cases of late-stage or unrelenting osteoporosis & in consultation with an integrated doctor the following can be considered
The use of a herbal supplement Pueraria mirifica (aka Krau krua) has been shown in animal studies, and human anecdotal/traditional, to be of benefit in osteoporosis and be safe to use - https://www.verywellhealth.com/the-benefits-of-pueraria-mirifica-88654 and https://www.ncbi.nlm.nih.gov/pubmed/18313241
Red Sage 500 mgs caps (100) http://cbr.ubc.ca/potential-anti-osteoporosis-drug-derived-from-a-traditional-medicinal-herb/
Bioidentical HRT (progesterone, oestrogen, testosterone)
As discussed above, this was a format of therapy promoted in the 1990s but as artificial progesterone (progestins) was too toxic, studies seemed to dry up in favour of oestrogen therapies. With the availability now of bHRT we can re-visit the therapy. We can go on to the use of bHRT Oestrogen (and testosterone) but there is a slight risk of reintroducing periods in women and creating feminising effects in men (breast growth).
Chelation if metal toxicity found (17).
References
-
http://www.dimond3.org/Dublin 2006/2 DEXA QA Training for Physicists/7 Accuracy of DEXA & other methods.pdf
- Med Sci Sports Exerc. 2013 Jan;45(1):178-85. doi: 10.1249/MSS.0b013e31826c9cfd. Effects of exercise sessions on DXA measurements of body composition in active people. Nana A1, Slater GJ, Hopkins WG, Burke LM
- Hernandez, CALCIFIED TISSUE INTERNATIONAL Volume 74, Number 4, 357-365.
- (Nephrol. Dial. Transplant. (1999)14 (8): 1917-1921)
- Nelson H, et al. Portland: Oregon Health & Science University Evidence-based Practice Center; 2001).
- (J Bone Miner Res. 2005 Oct;20(10):1813-9. Epub 2005 Jun 20 and Journal of Bone and Mineral Research Volume 13, Issue 2, pages 297–302, February 1998)
- Lehrer S, Montazem A, Ramanathan L, et al J Oral Maxillofac Surg. 2009 Jan;67(1):159-61. doi: 10.1016/j.joms.2008.09.015. and https://www.drweil.com/health-wellness/body-mind-spirit/bone-joint/beware-of-bone-boosters/
- (Osteoporos Int. 2007 Aug;18(8):1023-31).
- (Journal of the American Medical Association 23rd Feb 2011),
- BMJ 2010;341:c4444)
- (McCullagh 1969).
- http://www.sciencebasedmedicine.org/calcium-supplements-and-heart-attacks-more-data-more-questions/
- http://www.osteoporosis.ca/news/press-releases/new-vitamin-d-guidelines/
-
http://www.johnleemd.com/store/pgattack.html
- Osteoporosis and Stress Kumano H, Clin Calcium. 2005 Sep;15(9):1544-7. http://www.ncbi.nlm.nih.gov/pubmed/16137956
-
http://saveourbones.com/osteoporosis-milk-myth/
- Malmir H, Larijani B, Esmaillzadeh A. Consumption of milk and dairy products and risk of osteoporosis and hip fracture: a systematic review and Meta-analysis. Crit Rev Food Sci Nutr. 2020;60(10):1722-1737. doi: 10.1080/10408398.2019.1590800. Epub 2019 Mar 26. PMID: 30909722.
- Exercise for Osteoporosis - Is Walking Enough? Swezey, Robert L., M.D., Spine, 1996;21:2809-2813
- http://saveourbones.com/osteoporosis-milk-myth/
- Various papers on associations of metal with osteoporosis - https://scholar.google.co.uk/scholar?q=chelation+in+osteoporosis&hl=en&as_sdt=0&as_vis=1&oi=scholart&sa=X&ved=0ahUKEwianPL-gLTNAhXsK8AKHdMiBWYQgQMIGjAA





